Decoding Surgical Ablation Lesion Sets: The Headwind Standing Between Patients and Normal Sinus Rhythm
Every year thousands of patients with atrial fibrillation (AF) undergo mitral valve repair, CABG, or other open-heart procedures, and the OR becomes their once-in-a-lifetime opportunity to restore sinus rhythm — their one chance to break the cycle of AF progression, stroke risk, and worsening heart failure. But in that critical moment, when ablation could be performed, one question creates a massive headwind:
Which lesion set is right for this patient?
Not all cardiac surgery patients with AF are the same — and surgeons know this better than anyone and when it comes to surgical ablation (SA), the message delivered to the community over the years has been… confusing at best, and sometimes paralyzing.
And here’s the honest frustration:
More options and changes over time made that decision harder, not easier.
For several years, the message was clear:
“Do a full Cox-Maze IV— it’s the gold standard.”
Then shifted to:
“This alternative lesion set is good enough… sometimes.”
All of the updates were made with the best intentions and advanced based on new learning and data. But, the field was moving so quickly that it could be challenging to keep up.
New data, new guidelines, evolving techniques — it also made it appear like there wasn’t consensus. The result? A growing sense many surgeons quietly relate to:
If the specialists can’t decide, how am I supposed to?
Not because surgeons don’t want to treat AF, but because it can feel impossible to keep up with every lesion pattern and every new update. For some, it could feel like they shouldn’t participate in AF treatment at all. And this headwind is standing directly between patients and their best chance at sinus rhythm.
Why Lesion-Set Choices Matter
AF isn’t just an irregular heartbeat — it can profoundly impact patients:
- Reduced quality of life
- Increased stroke risk
- Contribution to heart failure
- Decreased long-term survival
From 2018 to 2020, approximately 103,382 Medicare beneficiaries with AF underwent cardiac surgery1 — each with a unique medical history. Data shows that when surgeons select the lesion set that best matches the patient:
- Sinus rhythm restoration rates increase
- Stroke and heart failure risks decrease
- Long-term survival improves
This is the BIG WHY – why choosing the right lesion set really matters for an AF patient.
The Challenge: Why Many Patients Miss Their Shot
The data is clear: the right ablation for the right patient changes lives. Yet, despite a Class I guideline recommendation, only about 1 in 5 eligible patients receive concomitant AF ablation and left atrial appendage occlusion (LAAO).1
Why? Surgeons face real obstacles:
- Longer cross-clamp and bypass times
- Complex lesion sets
- Increased risk of pacemaker need
- Renal complications
The question remains: how do we clear the path and choose the lesion set that works best for each patient?
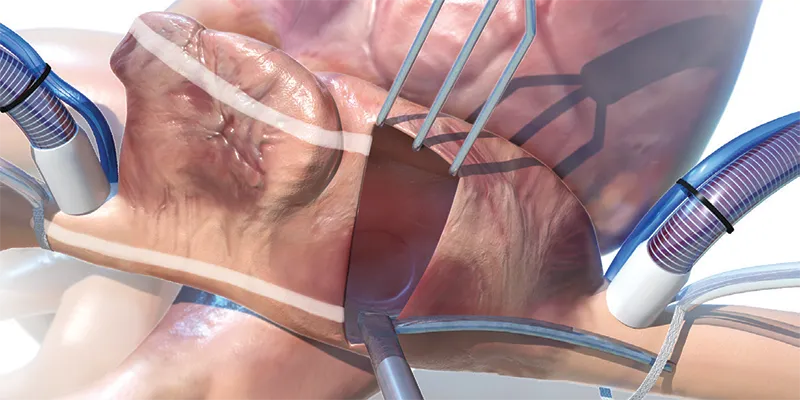
Matching the Ablation to the Patient
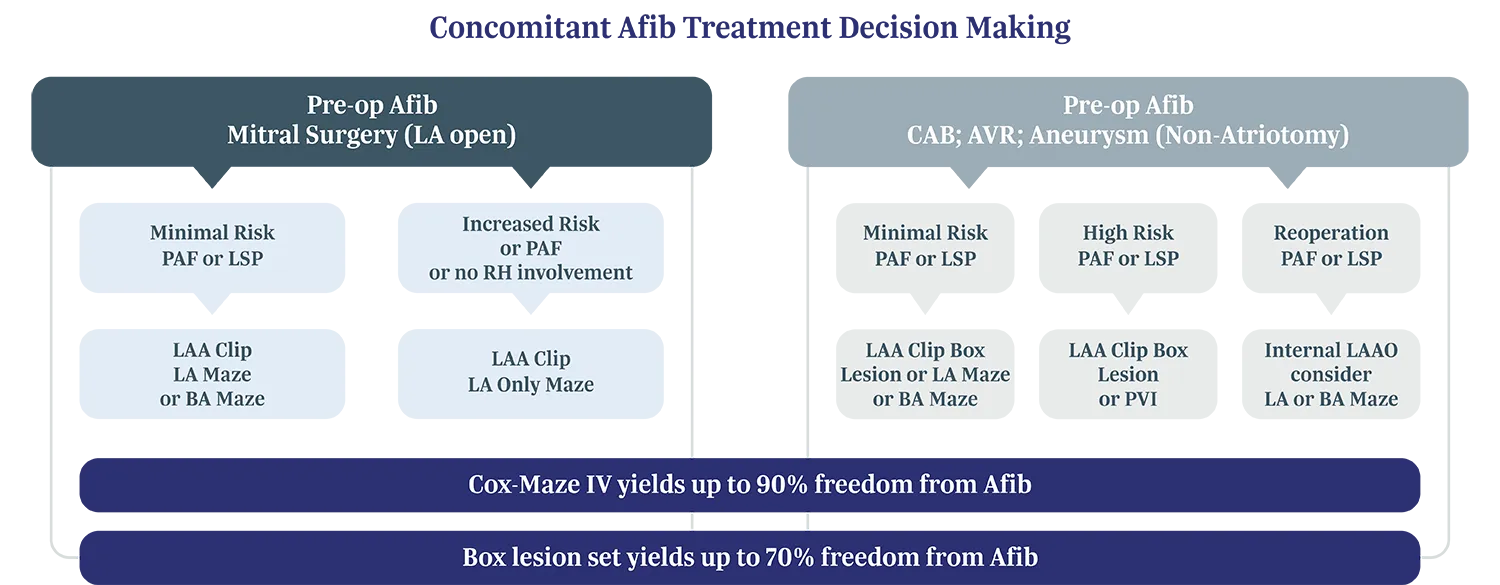
A recent article by Dr. McCarthy and Dr. Cox: "Practical approaches to concomitant surgical ablation of atrial fibrillation: Matching the ablation to the patient," provides a practical framework, emphasizing one central idea: effective AF treatment depends on tailoring the right lesion set for the patient, not a one-size-fits-all approach.
“The benefits of a perfect, complete, highly-effective SA operation have to be balanced with the reality of adding risk in complex surgical procedures in patients with comorbidities.”3
Dr. McCarthy and Dr. Cox’s paper highlights key factors that guide lesion-set selection:
- Type and duration of AF (paroxysmal, persistent, or long-standing)
- Left atrial size (larger atria may need more extensive lesions)
- Underlying heart disease
- Other surgical procedures being performed
They also provide a concise decision-making tree to help tailor ablation to the patient.
 *Image References
*Image References
Let’s break this decision tree down.
Step 1: LAAO is the minimum and should be considered for every patient with preop AF
- The LAAOS III trial of 4,770 AF patients showed that concomitant S-LAAO reduced the risk of late stroke or systemic embolism by 33% compared with patients who did not have LAA closure.5 Which means that many patients undergoing cardiac surgery could benefit, and it’s simple to do.
Step 2: What’s the index procedure? Atriotomy or Non-atriotomy.
Step 3: What’s the patient’s risk level? High or low.
Step 4: Match the ablation to the patient situation.
The options:
- Box lesion, Left atrial (LA) Maze, Bi-atrial (BA) Maze, PVI, or Posterior wall isolation
- Non-atriotomy: CABG, AVR
- Low risk Patient: Suitable for paroxysmal AF or smaller atria
- Typically includes pulmonary vein isolation and/or posterior wall isolation
- Shorter, simpler, and more effective when matched to patient needs
- Full Cox-Maze IV
- Atriotomy: Mitral valve
- High risk Patient: Best for long-standing AF or large atria
- Highest chance of restoring sinus rhythm
- More complex and time-intensive
Step 5: Do something: At the end of the day the data is clear – some treatment is better than no treatment. The final step in the decision process is for a surgeon to determine based on their experience what level of treatment they feel comfortable providing for the patient. This decision process could in some cases even include referring the patient back to the EP to confirm treatment success and support with additional catheter ablations.
“Also, the judgment has to be guided by the surgeons’ experience with the technologies and procedures. Surgeon experience is the most important factor influencing judgment.”4
– Patrick M. McCarthy, MD
The Takeaway
The intention to treat AF has never been stronger — patients deserve sinus rhythm. But without clarity, hesitation persists.
The good news? We’re closer than ever to eliminating that barrier – and the evidence is clear:
- Concomitant ablation improves rhythm control, survival, and stroke outcomes
- Modern techniques add minimal risk
- Outcomes are best when lesion sets are tailored to the patient
The future of AF surgery isn’t just performing ablation — it’s selecting the lesion set that fits each patient. Precision matters and restoring sinus rhythm should be part of every surgical plan when indicated.