Afib and Heart Failure Together: What Does It Mean, and What Can You Do?
For patients diagnosed with atrial fibrillation (Afib), there's something that’s not always fully apparent: Afib doesn't just affect your heart rhythm—it can lead directly to heart failure, which happens to be the leading cause of death in Afib patients.2
A Tale of Two Conditions That Encourage Each Other
Think of Afib and heart failure as partners that are up to no good. They don't just coexist—they actively make each other worse, creating what cardiologists call a "vicious cycle."1
How Afib Damages Your Heart
When the heart beats irregularly due to Afib, several negative things happen:
- Loss of coordinated pumping: The atria (upper chambers) stop contributing effectively to filling the ventricles
- Reduced filling time: The irregular, often rapid rhythm doesn't give your heart enough time to fill with blood
- Decreased cardiac output: Less blood gets pumped out to the body with each heartbeat
- Increased pressure: The backup effect increases pressure throughout your cardiovascular system
The Progression
This initial damage triggers the body's stress response systems, which can make things worse by:
- Stretching your left atrium
- Increasing atrial pressure and size
- Creating scar tissue (fibrosis) in your heart
- Generating more abnormal electrical triggers
- Slowing down normal electrical conduction
How does that progress? Afib gets worse, heart function deteriorates, and the cycle accelerates.
The Numbers That Tell the Story
The statistics surrounding Afib and heart failure are serious:
- After age 40: 1 in 4 people will develop Afib,6 and 1 in 5 will develop heart failure7
- Risk multiplier: Having Afib makes you 5 times more likely to develop heart failure10
- Mortality reality: 29% of Afib patients die of heart failure within a decade of diagnosis2
- Economic impact: Heart failure costs are expected to double to $70 billion by 20301
More importantly, these numbers represent millions of people whose lives could be improved with the right Afib treatment.
Hiding in Plain Sight – Shared Risk Factors
Part of what makes this relationship so dangerous is that Afib and heart failure often share the same underlying risk factors:9
- Hypertension
- Diabetes
- Obesity
- Sleep apnea
- Aging
- Genetics
- Chronic inflammation
This overlap means that by the time symptoms appear, both conditions may already be silently progressing.1
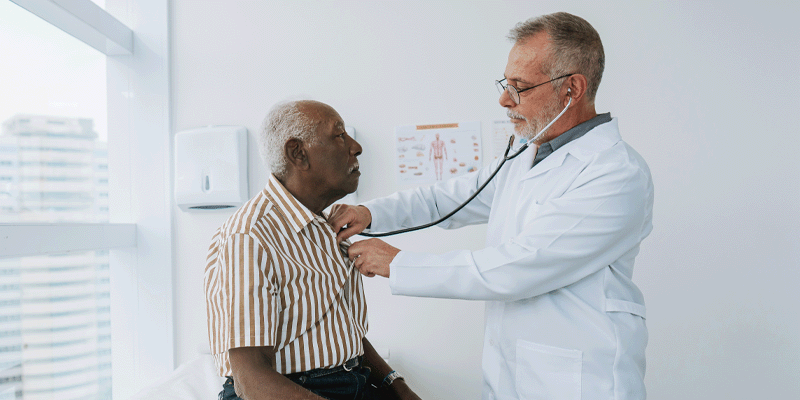
The Golden Opportunity: Surgical Intervention
There’s a great reason to be optimistic, though. For patients already having structural heart surgery—such as a valve repair or coronary artery bypass—that’s the golden opportunity to address Afib in the same procedure.
However, despite clear medical guidelines recommending Afib treatment during cardiac surgery and multiple studies showing the long-term survival benefits, Afib is ignored almost 80% of the time in patients already undergoing heart surgery.3-4 This represents thousands of missed opportunities each year to prevent future heart failure and improve patient outcomes.
The Evidence to Justify Acting
Research consistently shows that patients with Afib who receive surgical ablation during their cardiac procedure have:4, 11
- Improved long-term survival without increased surgical risk
- Better quality of life after surgery
- Return to normal life expectancy curves when sinus rhythm is restored
- Less functional impairment when they maintain normal rhythm8
What Restoring Normal Rhythm Means
When surgeons successfully restore normal heart rhythm by treating it during cardiac surgery, it’s similar to hitting the reset button on the Afib-heart failure cycle. Patients who spend more time in normal sinus rhythm experience:
- Improved exercise capacity
- Reduced hospitalizations
- Better overall heart function
- Decreased stroke risk
- Enhanced quality of life
Most importantly, treating Afib surgically can put patients back on the same life-expectancy curve as if they never had Afib in the first place.11
Breaking the Cycle: What Patients Can Do
Before Surgery
If you're scheduled for cardiac surgery and have Afib:
- Ask specifically about concurrent Afib treatment
- Request consultation with an electrophysiologist if your surgeon seems hesitant
- Understand the risks of leaving Afib untreated versus treating it
- Advocate for yourself—you may need to be persistent
Conversation Starters:
- "I understand Afib increases my risk of heart failure. Is it possible to address both issues during my surgery?"
- "What are the long-term consequences if we don't treat my Afib now?"
- "Can you explain any reasons why surgical Afib treatment might not be recommended in my case?"
The Bigger Picture: A Healthcare System Challenge
The undertreatment of Afib during cardiac surgery also represents a broader healthcare challenge. Despite strong evidence and clear guidelines, implementation remains inconsistent. This may be due to:
- Perceived complexity of the additional procedure
- Concerns about operative time
- Unfamiliarity with newer ablation techniques
- Focus on the primary surgical indication
However, these barriers can be small compared to the long-term consequences of leaving Afib with the patient.
Looking Forward: The Next 50 Years
Some medical experts have predicted that Afib and heart failure will dominate cardiovascular care for the next half-century.8 As our population ages and traditional risk factors become more prevalent, the importance of addressing these conditions together—not separately—will continue to grow.
Capitalizing on the Golden Opportunity
The vicious cycle created by Afib and heart failure together creates a call to action. Every day that Afib goes untreated, it's potentially accelerating damage to the heart and reducing cardiac output.
The good news? There are proven treatments that work.
The challenge? Working together to make sure they're offered and utilized.
If you have Afib or responsible for a patient with Afib are facing cardiac surgery, don't let this golden opportunity pass by to stop the progression.
Dr. Whitlock explains how establishing normal sinus rhythm has benefits in terms of heart failure outcomes.
PM-US-3652B-1026-G